I see a lot of patients with digestive complaints; some with heart burn, others with bloating and indigestion and still others dealing with chronic constipation or loose stool.
Insufficient stomach acid production is an often overlooked condition in many people complaining of digestive issues. Instead of finding the root cause, symptoms are addressed with band-aid treatments. If you have heartburn, you are prescribed an antacid (which further lowers your stomach acid levels). If you have IBS this is treated with fiber, laxatives and sometimes an antidepressant. If you have SIBO you are treated with an antibiotic. If you have food sensitivities, you are told to remove this food…. but none of these Band-Aids fix the root cause of the issue. If we look at each of these symptoms and conditions, most of these cases have something in common and that is low stomach acid.
"Reading a great post on Clean & Lean Revolution"
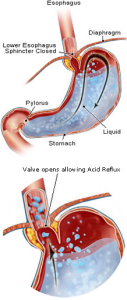
↑ Tweet ThisHeart Burn is Often Caused By Low Acidity
I know that this sounds counterintuitive, but here’s why: If you are not producing sufficient stomach acid then you will not digest your food at a quick enough clip. You need to have adequate stomach acidity to signal the sphincter to close between your stomach and your esophagus. If you don’t have the right stomach pH, then the sphincter won’t close and this will allow the stomach contents to back up into the esophagus, causing heart burn.
 Without sufficient stomach acids, food will not digest well enough. You won’t be able to break food down to the degree that you can access enough nutrition. This sends intact pieces of food into your digestive tract, which can lead to food sensitivities. Yes, removing a known food allergen is a good idea, but, if the underlying condition is not treated, you will likely become sensitive or allergic to another food.
Without sufficient stomach acids, food will not digest well enough. You won’t be able to break food down to the degree that you can access enough nutrition. This sends intact pieces of food into your digestive tract, which can lead to food sensitivities. Yes, removing a known food allergen is a good idea, but, if the underlying condition is not treated, you will likely become sensitive or allergic to another food.
If you aren’t digesting your foods well enough in your stomach, un-digested carbohydrates are fermented by gut flora causing bloating, cramping and sometimes diarrhea and sometimes constipation leading to IBS symptoms. Stomach acids, along with bile acids keep the flora in check at the beginning of the small intestine. When stomach acid is too low, this allows larger levels of flora and other organisms to take up residency in the upper small intestine, leading to SIBO, a small intestinal bacteria overgrowth.
Low stomach acid production has been directly linked to metabolic conditions and even rheumatoid arthritis – when intact pieces of food pass into the blood stream and settle in joints, the immune system can respond by attacking the area around the joints.
Why do some people produce too little stomach acid?
Low stomach acid is linked to hypothyroidism, autoimmune disorders, the use of antacids or proton pump inhibitors, stress, H.pylori, post cancer treatment that includes radiation, it is linked to gastritis – gut inflammation, if you have had gastric bypass you will be at risk. If you have a nutritional deficiency of niacin, zinc or iodine this will all affect stomach acid production.
Let’s get back to talking about the implications of not being able to digest your food. One question I ask in the intake session is ‘do you see any intact pieces of food in your stool.’ This often gets the reply, ‘no, only corn.’ On other occasions, the patient will reply, ‘yes, often.’ Intact pieces of food in your stool, yes, corn and anything else, is a serious symptom. Food is making it through every stage of digestion, un-digested. This may mean that you aren’t chewing well enough, your aren’t producing enough stomach acids or digestive enzymes, it may mean all of these and that there is inflammation or dysbiosis present (an imbalance in gut flora) and it may mean something more serious. As a nutrition detective, it is my job to figure out where the system is breaking down and to help you bring it back into balance.
Should You Supplement?
One of the things that we assess is whether or not you are producing enough stomach acids and whether you may need supplementation or support to produce sufficient stomach acids. A hydrochloric acid or HCL supplement, is an option. When you take this supplement, you aren’t taking enough to change the pH of your stomach. You are simply taking a very small dose that will help to digest the food that it is taken with. It has been shown in studies that taking a hydrochloric acid supplement does not suppress your body’s ability to make HCL. Which is a good thing, because we definitely don’t want to override your body’s ability to produce HCL naturally.
When is HCL Not a Good Idea?
If you have gastritis or an ulcer or a history of these – HCL is going to be contraindicated. You should always take HCL under the care of a qualified practitioner.
Another option is to take bitters. Bitter herbs help to stimulate the stomach to produce more acid. Bitter melon and gentian tea are two widely used bitters. Herbs are also bitters. I always recommend that at least one fresh herb is added to each meal (whether cilantro to a wrap, basil to a salad or chives and parsley to a stir fry).
The bitter taste gets the salivary glands going. It helps the stomach start secreting juices. The bitterness sends the signal to the brain to get the whole digestive tract—the liver, the pancreas, and the intestines—on the lookout for incoming food. One contributing factor to the epidemic issues that we are seeing with digestion is because we have bred the bitter out of food. But this is a topic for another video.
Angela Pifer, Certified Nutritionist
Work one on one with Seattle Nutritionist Angela through her private practice at www.NutritionNorthwest.com
Enjoying this content? Sign up for updates... It's FREE!

Comments
from 4 people
This is from a recent book that was published. I have had a patient try this and swear by it, though no other clinical evidence. I also don't recommend this for SIBO patients because celery is a high fermentable food.
Warmly
Angela
Angela
I have been hearing that celery juice has mineral salts and is alkaline which encourages your stomach to create more hydrocholoric acid on its own. Have you heard about this?
Linda
Hi Elizabeth, I am going to say 'yikes!!' here! I would never recommend a liquid HCL betaine. Not only are you worried about your teeth, you should also be worried about the lining of the esophagus, which is not at all used to acid. When I work one on one with patients, if warranted, I have them do an HCL challenge, where we test the need for this out. You can find digestive enzymes that have a little HCL in them, and this may be the baseline for most people.
Without enough HCL digestion, at all levels will be impacted, as well as you'll lack the ability to sterilize the food that you eat, so you will be more prone to gut imbalances. Low HCL is one risk factor for SIBO and a risk factor for SIBO reoccurrence.
If you find that you would like additional support - I do work long distance.
Warmly,
Angela
Angela
Regarding HCl supplements. I have an old-ish nutrition book by Adelle Davis called Let's Get Well. She says that HCl is a crutch - and a good crutch, too. In order to encourage your body produce its own HCl, it has to be able to break down & assimilate certain nutrients, esp. minerals & protein. But if you are low in HCl, you can't do this. Catch-22.
So she would advise her clients to take HCl supplements and in her day (1950s & 60s) it wasn't easy to do; you had to take it in liquid form and be careful with it not getting on your teeth. Alternatively, in that era, you would have to take large numbers of tablets. She also mentioned bitter foods.
She also knew an orthopedic specialist who had all his patients take a gastric juice analysis test. I wonder if the doctors today do this or not.
Adelle Davis is not the final word in nutrition, but I can say for sure it is a primary source that can lead you to more info.
Thank you. I'll bet you have carloads of clients, you seem to know a lot - more than most doctors.
Elizabeth
Leave A Comment